What is Diabetes?
Diabetes is a chronic medical condition that occurs when the body is unable to properly regulate blood sugar levels in the bloodstream. This happens when the pancreas either does not produce enough insulin (type 1 diabetes) or the body becomes resistant to the insulin it does produce (type 2 diabetes).
Untreated diabetes can lead to serious health complications such as cardiovascular disease, kidney disease, blindness, and other risks, including death,
Diabetes Symptoms
The most common symptoms of the onset of diabetes include:
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow healing of cuts and bruises
If you experience these symptoms, it’s important to see a doctor immediately for proper testing and diagnosis.
The Main Differences Between Type 1 and Type 2 Diabetes
There are many differences between type 1 diabetes (often referred to as Juvenile Diabetes) and type 2 diabetes.
Cause:
- Type 1 diabetes is an autoimmune disorder where the body mistakenly attacks and destroys the insulin-producing cells in the pancreas.
- Type 2 diabetes is caused by insulin resistance, where the body does not use insulin effectively, coupled with the pancreas not producing enough insulin.
Onset:
- Type 1 diabetes often develops in childhood or adolescence, though it can occur at any age.
- Type 2 diabetes typically develops later in life, often in adulthood.
Insulin Production:
- In type 1 diabetes, the pancreas produces little to no insulin.
- In type 2 diabetes, the pancreas may still produce insulin, but the body is unable to use it effectively.
Treatment:
- Type 1 diabetes requires insulin therapy, as the body cannot produce its own insulin.
- Type 2 diabetes is often initially treated with lifestyle changes, such as diet and exercise. Oral medications or insulin may be added if needed.
Risk Factors:
- Type 1 diabetes is not directly related to lifestyle factors.
- Type 2 diabetes is strongly linked to obesity, poor diet, and lack of physical activity.
Prevalence:
- Type 1 diabetes accounts for around 5-10% of all diabetes cases.
- Type 2 diabetes accounts for around 90-95% of all diabetes cases.
In summary, the primary differences between type 1 and type 2 diabetes lies in the underlying cause, age of onset, insulin production, and treatment approaches. Understanding these differences is crucial for proper diagnosis and management of the two types of diabetes.
Can Diabetes be Reversed?
In some cases, type 2 diabetes can be reversed through lifestyle changes. This typically involves losing weight through a healthy diet and regular exercise.
While type 1 diabetes cannot be reversed, its symptoms can be managed through insulin therapy and other treatments.
How to Prevent Type 2 Diabetes
The best way to prevent type 2 diabetes is to maintain a healthy lifestyle. This includes:
- Maintaining a healthy weight
- Eating a diet rich in whole, unprocessed foods
- Exercising regularly
- Limiting sugary and high-carb foods and beverages
- Getting enough sleep
- Managing stress
By making these lifestyle changes, you can significantly reduce your risk of developing type 2 diabetes.
Managing Diabetes

Managing diabetes requires a multi-pronged approach, including:
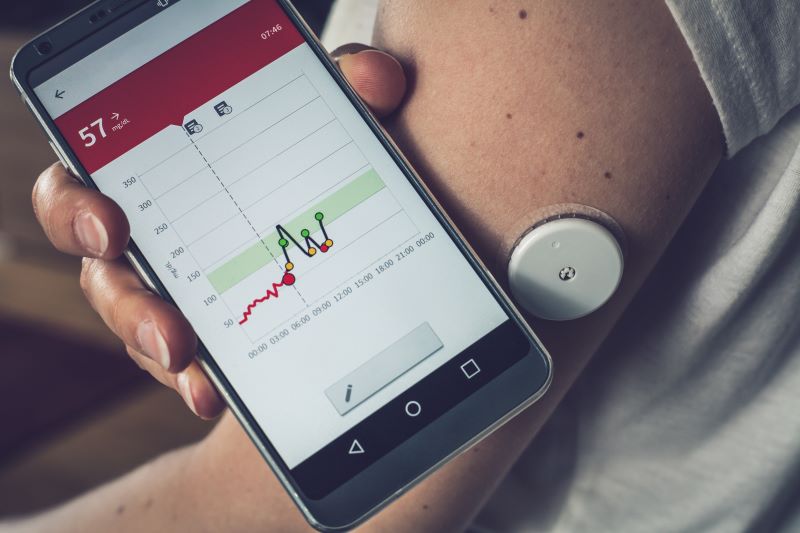
- Monitoring blood sugar levels
- Taking medication as prescribed
- Eating a healthy, balanced diet
- Engaging in regular physical activity
- Managing stress
With proper management, people with diabetes can live long, healthy lives.
How to Manage Food as a Diabetic

For those with type 2 diabetes, it’s important to limit foods that are high in refined carbs, added sugars, and unhealthy fats. This includes things like:
- Sweets and desserts
- White bread, pasta, and rice
- Sugary drinks like soda and juice
- Fried and processed foods
Instead, type 2 diabetics should focus on eating plenty of lean proteins, non-starchy vegetables, whole grains, and healthy fats such as olive oil.
Individuals with type 1 diabetes also need to be mindful about the quantity and timing of eating certain foods. Here are some key dietary considerations for type 1 diabetics:
Carbohydrates:
- Carbs have the biggest impact on blood sugar levels for type 1 diabetics.
- They need to carefully count and monitor carb intake at each meal and snack.
- Restricting high-carb foods like sugary drinks, desserts, and refined carbs is important.
Fiber:
- Eating fiber-rich foods like vegetables, fruits, and whole grains can help slow the absorption of carbs.
- This can lead to more stable blood sugar levels.
Protein and healthy fats:
- Balancing meals with protein and healthy fats can also help manage blood sugar.
- Foods like lean meats, fish, nuts, and oils are good choices.
Alcohol:
- Alcohol can affect blood sugar levels, so type 1 diabetics need to be cautious.
- They should only drink in moderation and monitor their levels carefully.
Timing of meals and insulin:
- Coordinating insulin dosing with meal timing is critical for type 1 diabetics.
- The key is finding the right balance of carbs, protein, and fats to maintain stable blood sugar levels. Working closely with a healthcare team is important for developing a personalized meal plan.
Diabetes and Mental Health

Dealing with a chronic condition like diabetes can take a heavy toll on mental health. People with diabetes are at a higher risk of developing depression and anxiety. It’s important to prioritize self-care and seek support when needed.
Managing mental health is just as important for people with diabetes as managing their physical health. Here are some tips for how people with diabetes can proactively care for their mental well-being:
Seek Professional Support:
- Consider working with a mental health professional, such as a therapist or counselor, who specializes in treating people with chronic conditions.
- They can provide counseling, coping strategies, and treatment for conditions like depression or anxiety.
Join a Support Group:
- Connecting with others who understand the daily challenges of living with diabetes can provide invaluable emotional support.
- Look for in-person or online diabetes support groups.
Practice Stress Management:
- Find healthy ways to manage stress, such as through meditation, yoga, deep breathing, or engaging in hobbies.
- Chronic stress can negatively impact blood sugar levels.
Prioritize Self-care:
- Make time for activities that bring joy and relaxation, such as reading, taking a bath, or going for a walk.
- Ensure you’re getting enough sleep, eating a balanced diet, and staying physically active.
Communicate Openly:
- Have open discussions with your healthcare team about your mental health concerns.
- Work together to develop a comprehensive treatment plan that addresses both your physical and mental well-being.
Consider Medication If Needed:
- In some cases, antidepressants or other psychiatric medications may be helpful in managing mental health conditions related to diabetes.
- Work closely with your doctor to determine the right treatment approach.
Prioritizing mental health is crucial for people with diabetes to better manage their condition, improve quality of life, and achieve optimal overall health.
Dealing with a chronic condition like diabetes can take a heavy toll on mental health. People with diabetes are at a higher risk of developing depression and anxiety. It’s important to prioritize self-care and seek support when needed.
Managing mental health is just as important for people with diabetes as managing their physical health. Here are some tips for how people with diabetes can proactively care for their mental well-being:
Seek Professional Support:
- Consider working with a mental health professional, such as a therapist or counselor, who specializes in treating people with chronic conditions.
- They can provide counseling, coping strategies, and treatment for conditions like depression or anxiety.
Join a Support Group:
- Connecting with others who understand the daily challenges of living with diabetes can provide invaluable emotional support.
- Look for in-person or online diabetes support groups.
Practice Stress Management:
- Find healthy ways to manage stress, such as through meditation, yoga, deep breathing, or engaging in hobbies.
- Chronic stress can negatively impact blood sugar levels.
Prioritize Self-care:
- Make time for activities that bring joy and relaxation, such as reading, taking a bath, or going for a walk.
- Ensure you’re getting enough sleep, eating a balanced diet, and staying physically active.
Communicate Openly:
- Have open discussions with your healthcare team about your mental health concerns.
- Work together to develop a comprehensive treatment plan that addresses both your physical and mental well-being.
Consider Medication If Needed:
- In some cases, antidepressants or other psychiatric medications may be helpful in managing mental health conditions related to diabetes.
- Work closely with your doctor to determine the right treatment approach.
Prioritizing mental health is crucial for people with diabetes to better manage their condition, improve quality of life, and achieve optimal overall health.
At Catawba Valley Healthcare, primary care providers, psychiatrists, therapists and social workers all work together under one roof towards one goal: whole person, integrated, patient care. At CVH, providers take the biopsychosocial, whole person model of healthcare seriously in order to practice what they believe is the best model for healthcare delivery for all of their patients.

